Study: Is the cardiovascular system a therapeutic target for cannabidiol?
Study: Is the cardiovascular system a therapeutic target for cannabidiol?
Christopher P Stanley, William H Hind, and Saoirse E O’Sullivan
Abstract
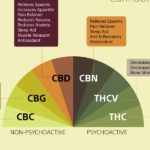
Cannabidiol (CBD) has beneficial effects in disorders as wide ranging as diabetes, Huntington’s disease, cancer and colitis.
Accumulating evidence now also suggests that CBD is beneficial in the cardiovascular system.
CBD has direct actions on isolated arteries, causing both acute and time-dependent vasorelaxation. In vitro incubation with CBD enhances the vasorelaxant responses in animal models of impaired endothelium-dependent vasorelaxation. CBD protects against the vascular damage caused by a high glucose environment, inflammation or the induction of type 2 diabetes in animal models and reduces the vascular hyperpermeability associated with such environments. A common theme throughout these studies is the anti-inflammatory and anti-oxidant effect of CBD.
In the heart, in vivo CBD treatment protects against ischaemia-reperfusion damage and against cardiomyopathy associated with diabetes. Similarly, in a different model of ischaemia-reperfusion, CBD has been shown to reduce infarct size and increase blood flow in animal models of stroke, sensitive to 5HT1A receptor antagonism.
Although acute or chronic CBD treatment seems to have little effect on haemodynamics, CBD reduces the cardiovascular response to models of stress, applied either systemically or intracranially, inhibited by a 5HT1A receptor antagonist.
In blood, CBD influences the survival and death of white blood cells, white blood cell migration and platelet aggregation. Taken together, these preclinical data appear to support a positive role for CBD treatment in the heart, and in peripheral and cerebral vasculature. However, further work is required to strengthen this hypothesis, establish mechanisms of action and whether similar responses to CBD would be observed in humans.
Additional Quotes from the body of the study:
In this paper, CBD was shown to antagonize the vasorelaxant effects of Abn-CBD and AEA. Begg et al. [26] showed in human umbilical vein endothelial cells (HUVECs) that Abn-CBD causes hyperpolarization through PTX-sensitive activation of large conductance calcium activated potassium channels (BKCa).
Similarly, in rat isolated mesenteric arteries, Abn-CBD causes vasorelaxation that is dependent on the endothelium, SR141716A sensitive pathways and potassium channel hyperpolarization through large, intermediate and small conductance calcium activated potassium (BKCa/IKCa/SKCa) channels [27].
More recently it has been shown that Abn-CBD causes vasorelaxation in the human pulmonary artery through similar mechanisms [29]. Taken together, these findings offer support to the presence of an endothelial bound Gi/o protein coupled receptor that causes vasorelaxation through hyperpolarization that is activated by Abn-CBD.
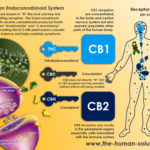
In human mesenteric arteries, we have very recently shown that CBD causes vasorelaxation of U46619 and endothelin-1 pre-constricted arterial segments (Stanley & O’Sullivan, 2012, under review). In human mesenteric arteries, CBD-induced vasorelaxation has a pEC50 in the mid-micromolar range which is similar to that observed in rat mesenteric arteries. However, CBD-induced vasorelaxation in human arteries has a maximal response of ∼40% reduction of pre-imposed tone. We went on to show that CBD-induced vasorelaxation in human mesenteric arteries is endothelium-dependent, involves CB1 receptor activation and TRPV channel activation, nitric oxide release and potassium hyperpolarization (Figure 1) (Stanley & O’Sullivan, 2012, under review).
CBD is known to be anxiolytic. CBD treatment reduces anxiety related to public speaking or fearful stimuli in humans [10]. A number of studies have now also shown that CBD reduces the cardiovascular response to anxiety or stressful situations. Resstel and colleagues have shown in Wistar rats that a single dose of CBD (10 or 20 mg kg−1 i.p.) reduced the heart rate and blood pressure response to conditioned fear [49] or to acute restraint stress [48]. The inhibitory effect of CBD on the cardiovascular response to stress was shown to be inhibited by WAY100635, a 5HT1A receptor antagonist. This effect appears to be mediated in the brain, as the same effect of CBD on cardiovascular responses could be mimicked when CBD was injected into the bed nucleus of the stria terminalis (a limbic structure) [50]. The potential ability of CBD treatment in humans to reduce the cardiovascular (as well as behavioural) response to stress could have significant effects on the development of atherosclerosis and hypertension, which are known to be accelerated by stress [51, 52].
There is a growing body of evidence that administration of CBD can ameliorate the negative effects of conditions associated with endothelial dysfunction. The high glucose conditions associated with diabetes have been reported as a causal factor in endothelial dysfunction. High glucose promotes inhibition/uncoupling of endothelial nitric oxide, increased superoxide production, increased actions of constrictor prostanoids, decreased actions of vasorelaxant prostanoids and increased reactive oxygen species [59]. Alongside these changes, high glucose is also reported to increase leucocyte adhesion and monocyte endothelial migration [60], which has been reported to be through NFκB activity [61].
Find the full study here http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3579247/